Abstract
Background: SCT is a standard therapeutic approach for patients with MM and has contributed to improved outcomes. While SCT utilization in MM has increased for all racial-ethnic subgroups over time, population-based studies have repeatedly shown that racial minorities are less likely to receive it. We explored factors that determine SCT utilization among patients within a given race to understand intra-racial disparities and how to address them in order to maximize the use of this imperative treatment among eligible patients.
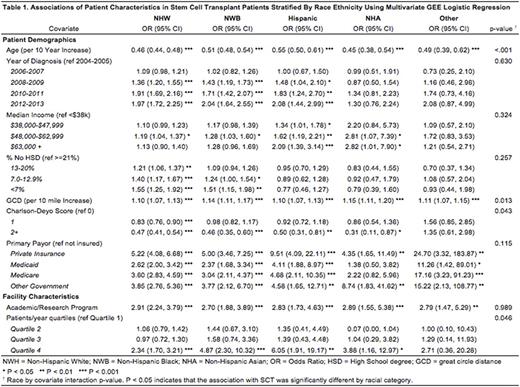
Methods: The 2016 National Cancer Database (NCDB) for MM with patients diagnosed between 2004-2013 was studied. Cases without information on the selected patient or facility characteristics evaluated in this analysis, including SCT use, race, median income, insurance status or facility type of initial MM diagnosis and/or treatment were excluded. The association between utilization of SCT as part of initial therapy of MM and socio-demographic factors was studied stratifying patients into mutually exclusive racial-ethnic subgroups non-Hispanic Whites (NHW), non-Hispanic Blacks (NHB), Hispanics, non-Hispanic Asians (NHA) and others using multivariate GEE logistic regression analysis (clustered on facility ID). Interactions between race and patient/facility characteristics and SCT utilization were tested using similar methods but including all races.
Results: Of the 123480 unique MM patients in NCDB diagnosed between 2004-2013, 111799 met the inclusion criteria. Of these, 15021 patients (13.4%) received SCT as part of initial MM therapy. Of those who received SCT, 77.5% were NHW (14.4% of all NHW), 15.1% NHB (10.3% of all NHB), 5.2% Hispanics (13.2% of all Hispanics), 2% NHA (15.5% of all NHA) and <1% others. There was no difference by gender but significantly reduced odds of receiving SCT were noted for every 10-year increase in age at diagnosis for all racial subgroups. NHA were the only subgroup not to have a significant year-wise increase over time in odds of receiving SCT between 2004-2013. A significant increase in SCT utilization was seen with increasing median income (quartiles; 2008-2012 data), for NHW and Hispanics but not for NHB and NHA, while increased education (% population with high-school degree; 2008-2012 data) was associated with a significant increase in SCT use for NHW and NHB, but not among Hispanics or NHA. An increase in great circle distance (GCD) from the treating facility as well as a lower Charlson-Deyo comorbidity index (CCI) was associated with significantly increased odds of receiving SCT for all racial groups. Insurancepayer status significantly affected odds of receiving SCT among all races with those having private insurance to be most likely to receive SCT among NHW, NHB and Hispanics while those with "other government" insurance payer type being most likely among NHA. Among treating facility characteristics, patients of all races were more likely to receive SCT if treated at an academic/researchfacility (including NCI-designated centers) or centers with highest quartile of patientvolume seen. For analysis by geographicalregion, NHW and NHA had the highest odds of receiving SCT in mountain region but there was no impact of geography on SCT for NHB or Hispanics. Odds ratio (OR) of receiving SCT as part of initial MM therapy by socio-demographic and facility characteristics for patients of individual racial subgroups are shown in Table 1. A significant interaction between odds of receiving SCT and various racial subgroups was noted for patient age at diagnosis (p<.001, decreased odds among NHW and NHA), GCD from treating facility (p=0.013, increased odds among NHB and NHA), CCI (p=0.043, decreased odds among NHA) and treatment facility volumes (p=0.046, increased odds among NHA and Hispanics).
Conclusions: In the largest analysis exploring socio-demographic factors affecting SCT utilization in MM we note a significant disparity within races for who gets SCT as a part of initial MM management and who does not. While some of these factors are non-modifiable, others including access to healthcare, income, insurance and literacy levels, proximity to treatment center, treating facility type as well as volumes are modifiable and appear to be barriers to SCT among in some races, while not in others. These must be addressed to minimize disparities within racial subgroups, especially the minorities and realize maximal benefit of SCT for MM.
Ailawadhi: Novartis: Consultancy, Honoraria; Pharmacyclics: Research Funding; Amgen: Consultancy, Honoraria; Takeda: Consultancy, Honoraria. Sher: LAM Therapeutics, Inc: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal